- Case Report
- Open access
- Published:
Unusual presentation and delayed diagnosis of cardiac angiosarcoma
Journal of Cardiothoracic Surgery volume 19, Article number: 161 (2024)
Abstract
Background
Primary cardiac angiosarcomas are very rare and present aggressively with high rates of metastasis. Given the poor prognosis, particularly once disease has spread, early diagnosis and multidisciplinary treatment is essential.
Case presentation
We present the case of a 46-year-old male who presented with chest pain, intermittent fevers, and dyspnea. Workup with computed tomography scan and transesophageal echocardiography demonstrated a right atrial pseudoaneurysm. Given the concern for rupture, the patient was taken to the operating room, where resection of the pseudoaneurysm and repair using a bovine pericardial patch was performed. Histopathology report initially demonstrated perivascular lymphocyte infiltrate. Six weeks later, the patient represented with chest pain and new word finding difficulty. Workup revealed multiple solid lung, pericardial, brain, and bone nodules. Eventual biopsy of a cardiophrenic nodule demonstrated angiosarcoma, and rereview of the original pathology slides confirmed the diagnosis of primary cardiac angiosarcoma.
Conclusions
Primary cardiac angiosarcomas are often misdiagnosed given the rarity of these tumors, but early diagnosis and initiation of treatment is essential. The unique presentation of our case demonstrates that clinical suspicion for cardiac angiosarcoma should be maintained for spontaneous pseudoaneurysm originating from the right atrium.
Background
Primary cardiac angiosarcomas are very aggressive tumors that often present after metastatic spread. Given the aggressive nature of the disease, early diagnosis is essential. We describe the case of a patient with primary cardiac angiosarcoma who initially presented with a right atrial pseudoaneurysm.
Case presentation
We present a case of 46-year-old male with no pertinent past medical history who presented to the emergency department with ongoing chest pain for 9 days associated with intermittent fevers and shortness of breath. On examination, the patient had a heart rate of 88 beats per minute and blood pressure of 143/72 mmHg. There were no audible murmurs or rubs on auscultation. He endorsed ongoing chest pain and shortness of breath.
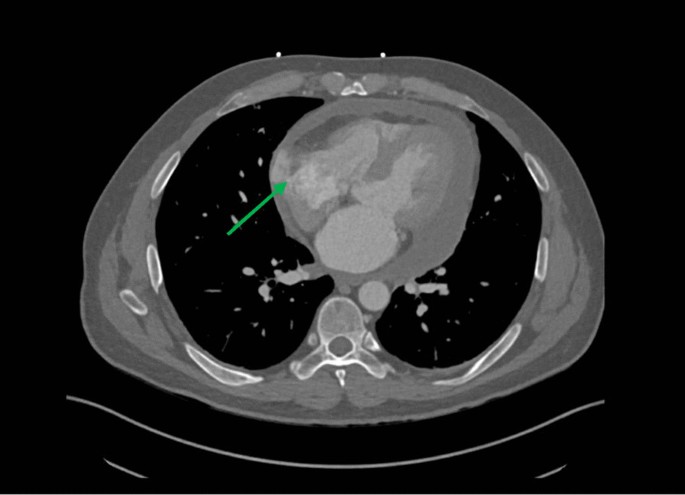
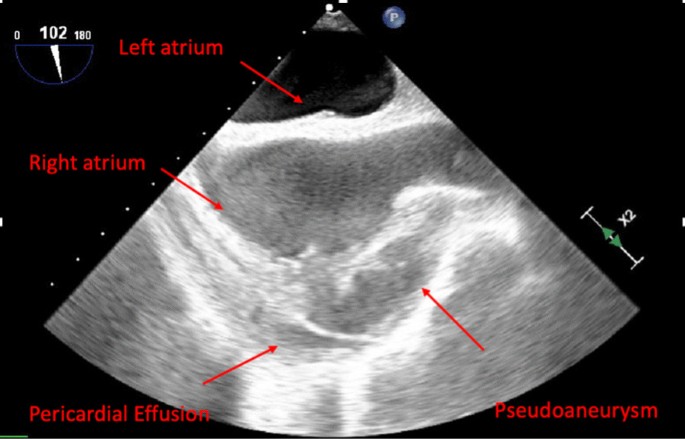
The patient underwent contrast computed tomography (CT) angiography pulmonary embolism with pulmonary arterial phase timing that showed no evidence of pulmonary embolism, but demonstrated a moderate sized pericardial effusion with high density concerning for hemopericardium, along with an outpouching on the right atrial wall with a narrow neck concerning for a pseudoaneurysm (Fig. 1). Further workup, including lab work and an electrocardiogram, were unremarkable. Transesophageal echocardiogram (TEE) redemonstrated the pericardial effusion and right atrial pseudoaneurysm (Fig. 2).
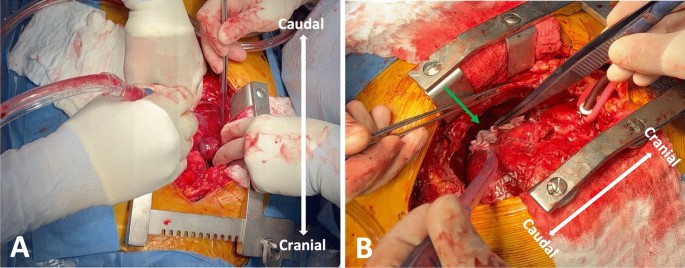
The case was discussed at the multidisciplinary cardiac conference and the decision was made to take the patient to the operating room given his ongoing symptoms as well as concern for hemopericardium and rupture of pseudoaneurysm into the pericardial space. Cardiac magnetic resonance imaging (MRI) and positron emission tomography (PET) CT were not performed given time-sensitive nature of the case and the desire for tissue diagnosis. The operation was performed via median sternotomy with cardiopulmonary bypass. A pericardial effusion and dense pericardial adhesions were found intraoperatively. After meticulous lysis of adhesions, central cannulation was performed, and the aorta and right atrium were cannulated. Right atrial pseudoaneurysm was identified (Fig. 3) and excised with the surrounding atrial wall. The defect in the atrial wall was closed using a bovine pericardial patch. Full exploration of the chest revealed no other lesions. The resected specimen was sent for pathology to try to establish tissue diagnosis and the patient was closed. The patient’s post-operative course was unremarkable, and he was discharged home on post operative day 4. Operative cultures showed no growth. Pericardial fluid cytopathology demonstrated abundant mixed inflammation with eosinophils, reactive mesothelial cells, histiocytes, and lymphocytes, with no malignant neoplasm identified. Tissue histopathology demonstrated granulation tissue, perivascular lymphocyte infiltrate, dense fibrous tissue, focal calcification, and organizing fibrin thrombus, but no evidence of malignancy.
Six weeks postoperatively, the patient presented to emergency department with chest pain, new word finding difficulty, clumsiness, gait instability, and intermittent low-grade fevers. A CT chest scan showed multiple halo-like solid lung, pericardial, and bone nodules (Fig. 4A, B). The CT head scan showed 1–1.5 cm left anterior thalamic and left temporal lobe hemorrhagic lesions. Magnetic resonance imaging of the brain demonstrated multiple enhancing lesions in the left temporal lobe, left anterior thalamus, and right parietal lobe (Fig. 4C). Together, the findings were suspicious for hemorrhagic metastasis, invasive fungal infection (such as invasive aspergillosis), or septic emboli. Given the concern for metastatic process, a biopsy of a lung nodule was performed and showed focal organizing exudative and fibrotic pneumonia negative for carcinoma. A lumbar puncture was also performed and showed no malignant neoplasm. Given the repeated surgical specimens that were negative for malignancy, an extensive infectious and rheumatologic workup was pursued. He was discharged with outpatient infectious disease follow-up, as the most likely diagnosis on the differential was thought to be invasive fungal infection and cultures would take several weeks to result.
Imaging findings on representation. A Computed tomography (CT) of chest showing multiple lung nodules (green arrows). B CT of chest showing nodular appearance of pericardial effusion and outpouching of the right atrium. C Head magnetic resonance imaging (MRI) demonstrating peripherally enhancing lesions (red arrow)
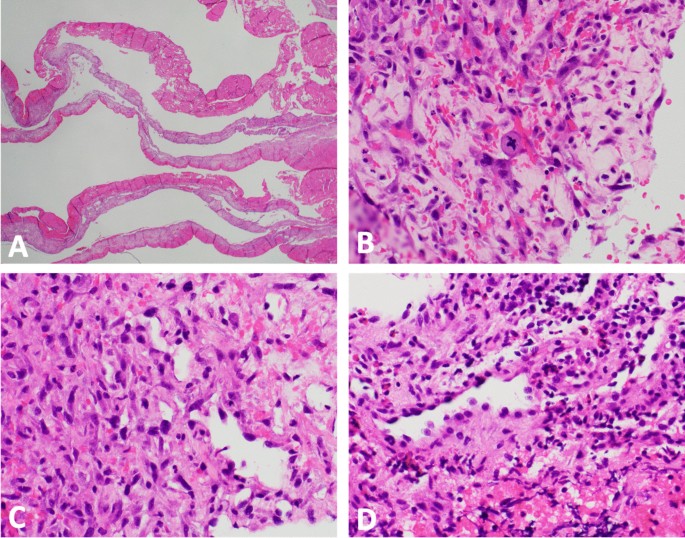
He represented one week later with returned right-sided chest pain, intermittent headaches, and abdominal pain. Repeat CT scan demonstrated increased number of pulmonary and pericardial nodules. Given the patient’s diagnostic dilemma and ongoing symptoms, a cardiophrenic nodule was biopsied with image guidance. Pathology demonstrated atypical cells, anaplasia, and poorly-formed vascular lumina, suggestive of angiosarcoma (Fig. 5).
Pathology findings demonstrating angiosarcoma. A low power magnification (× 12.5) hematoxylin and eosin staining of pseudoaneurysm reveals fibrin and organizing hematoma with a variably cellular fibrous cyst wall. B High power magnification (× 400) of pseudoaneurysm reveals scattered enlarged pleomorphic tumor cells with rare atypical mitoses in the background of abundant reactive granulation tissue. C Cardiophrenic nodule (× 400) shows similar atypical cells with unequivocal anaplasia and poorly-formed vascular lumina. D Cardiophrenic nodule (× 400) shows malignant endothelial cells with endothelial hobnailing into the vascular lumen
The patient’s tissue biopsy from his initial right atrial pseudoaneurysm resection was retrospectively reviewed and similar atypical cells were noted in the background of granulation tissue and organizing thrombus (Fig. 5). A diagnosis of primary cardiac angiosarcoma was made. The patient is currently undergoing chemotherapy with weekly paclitaxel for metastatic cardiac angiosarcoma.
Discussion and conclusions
Primary tumors of the heart are very rare and are identified in only 1 in 500 cardiac surgical cases. Of these, malignant tumors make up only 25%, the majority (95%) of which are cardiac sarcomas [1]. Angiosarcomas are the most common histologic subtype of cardiac sarcomas (30%) and are very aggressive in nature with high rates of metastasis [2].
Cardiac angiosarcomas more frequently present in males (2–3:1 male:female ratio) and most commonly arise from the right atrium [3]. Patients often present with nonspecific symptoms such as chest pain, dyspnea, weight loss, and fatigue [1]. Later in the disease course, patients may present with more specific symptoms, such as pericardial effusion, due to local infiltration into the myocardium and neighboring structures. Over half of patients present with metastatic disease, with spread to the lungs or pleura being most common [3]. Imaging can aid in the diagnosis of cardiac angiosarcomas. CT scan often shows a large multilobular mass that comprises the majority of the right atrium [4]. Transthoracic echocardiography (TTE) often shows a large echogenic mass with poorly defined borders and can be used to understand the size and location of the mass, understand its relation to other structures, and determine if cardiac function is affected [5]. Magnetic resonance imaging (MRI) can be used to differentiate between thrombus and tumor [6]. Histopathologically, angiosarcomas are difficult to diagnose due to the cellular heterogeneity. Common tumor markers include CD34, CD31, and factor VIII [1].
Due to the aggressive nature of this cancer, early diagnosis is essential. Our case represented a diagnostic challenge and initially presented on imaging as a right atrial pseudoaneurysm with a narrow neck, as opposed to a large multilobular mass with broad-based attachment typically described for cardiac angiosarcoma [4, 5]. Diagnosis was further delayed by the challenging histologic presentation in the context of low clinical suspicion, with malignant cells being obscured by extensive fibrin, granulation tissue, and organizing thrombus. Given these difficulties, diagnosis was not made until after distant metastatic spread and a cardiophrenic metastatic lesion was biopsied.
Given the rarity of this tumor and high mortality rate, there is no standardized approach to treatment. Without surgical resection, average survival is about 4 months [1]. The mainstay of treatment involves complete surgical resection, with a median post-operative survival of about 14 months [1, 3]. However, achieving complete resection with negative margins is often difficult given the diagnostic delay and proximity to vascular structures and propensity for distant microscopic spread at time of diagnosis. Chemotherapy and radiation are often used in the treatment either as neoadjuvant or adjuvant therapy, but the exact role of these modalities remains unknown [7, 8]. Overall, a multidisciplinary approach involving local resection, systemic chemotherapy, and radiation therapy seems to be the most favorable strategy.
Primary cardiac angiosarcomas are often misdiagnosed given the rarity of these tumors. Cardiac angiosarcoma presenting initially on imaging as either a right atrial pseudoaneurysm or a right coronary artery aneurysm has only been reported in a handful of case reports [9,10,11,12,13,14]. The unique presentation of this case demonstrates that clinical suspicion for cardiac angiosarcoma should be maintained for spontaneous pseudoaneurysm originating from the right atrium. With an aggressive disease course, early diagnosis is vital and allows for multidisciplinary care with medical and radiation oncology to offer patients the best chances of survival.
Availability of data and materials
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- TEE:
-
Transesophageal echocardiogram
- TTE:
-
Transthoracic echocardiography
References
Patel SD, Peterson A, Bartczak A, et al. Primary cardiac angiosarcoma—a review. Med Sci Monit. 2014;20:103–9. https://doi.org/10.12659/MSM.889875.
Ferguson PC. Surgical considerations for management of distal extremity soft tissue sarcomas. Curr Opin Oncol. 2005;17(4):366–9. https://doi.org/10.1097/01.cco.0000166651.38417.c8.
Look Hong NJ, Pandalai PK, Hornick JL, et al. Cardiac angiosarcoma management and outcomes: 20-year single-institution experience. Ann Surg Oncol. 2012;19(8):2707–15. https://doi.org/10.1245/s10434-012-2334-2.
Kassop D, Donovan MS, Cheezum MK, et al. Cardiac masses on cardiac CT: a review. Curr Cardiovasc Imaging Rep. 2014;7(8):9281. https://doi.org/10.1007/s12410-014-9281-1.
Luo L, Zhao W, Wang Y, Liu K. Cardiac angiosarcoma: a case report and review of the literature. Echocardiography. 2021;38(12):2083–90. https://doi.org/10.1111/echo.15221.
Riles E, Gupta S, Wang DD, Tobin K. Primary cardiac angiosarcoma: a diagnostic challenge in a young man with recurrent pericardial effusions. Exp Clin Cardiol. 2012;17(1):39–42.
Penel N, Bui BN, Bay JO, et al. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX study. JCO. 2008;26(32):5269–74. https://doi.org/10.1200/JCO.2008.17.3146.
Blackmon SH, Reardon MJ. Surgical treatment of primary cardiac sarcomas. Tex Heart Inst J. 2009;36(5):451–2.
Sawamura T, Takiya H, Yamada T, Sugimoto H, Kawai H. A case of cardiac angiosarcoma with a pseudoaneurysm formed in the right coronary artery. Kyobu Geka. 1994;47(7):565–8.
Serra V, Moura L, Almería C, Pérez de Isla L, Zamorano J. Right atrial rupture. Rev Port Cardiol. 2004;23(5):731–6.
Berry MF, Williams M, Welsby I, Lin S. Cardiac angiosarcoma presenting with right coronary artery pseudoaneurysm. J Cardiothorac Vasc Anesth. 2010;24(4):633–5. https://doi.org/10.1053/j.jvca.2009.04.002.
Chaturvedi A, Vummidi D, Shuman WP, Dubinsky TJ, Maki JH. Cardiac angiosarcoma: an unusual cause of coronary artery pseudoaneurysm. J Thorac Imaging. 2012;27(1):W8. https://doi.org/10.1097/RTI.0b013e3182078187.
Kimura S, Yonekura R, Umesue M. Angiosarcoma mimicking an infected pseudoaneurysm after graft replacement. Ann Thorac Surg. 2015;100(3):1114. https://doi.org/10.1016/j.athoracsur.2015.05.084.
Murthy JSN, Gorantla R, Periyasamy T, et al. Right atrial angiosarcoma presenting as giant pseudoaneurysm with impending rupture. IHJ Cardiovasc Case Rep. 2017;1(3):165–8. https://doi.org/10.1016/j.ihjccr.2016.09.002.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
SZ: Concept/design, drafting article, critical revision of article, approval of article. AZ: Drafting article, critical revision of article, approval of article. JG: pathological examination of the tumor sample, drafting of the article, critical revision of the article, and approval of the article. AK: Concept/design, critical revision of article, approval of article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent was obtained from the patient for the publication of this report.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zaheer, S., Zhou, A.L., Gross, J.M. et al. Unusual presentation and delayed diagnosis of cardiac angiosarcoma. J Cardiothorac Surg 19, 161 (2024). https://doi.org/10.1186/s13019-024-02555-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-024-02555-8